Vertical Transmission infections [TORCH]
Vertical Transmission infections
“vertically transmitted infection is
an infection caused by pathogens (such as bacteria and viruses) that use
mother-to-child transmission.”
Types of infections:
Several
vertically transmitted infections are included in the
“TORCH
complex”
T – toxoplasmosis from Toxoplasma gondii
O – other infections (see below)
R – rubella
C – cytomegalovirus
H – herpes simplex virus-2 or neonatal herpes simplex
Vertical transmission
of pathogens:
Babies born
of pregnant women who are infected with a particular virus are at risk of
contracting that virus from the parent. Transmission is more likely when the
baby is in direct contact with the mother’s fluids, such as during
breastfeeding and also in utero if there are breaks in the placental barrier,
although most vertical transmissions occur during delivery.
Multiple types of virus can be passed from mother to child via vertical transmission, including those known as “TORCH” pathogens: toxoplasma gondii, other (listeria monocytogenes, treponema pallidium, parvovirus, HIV, varicella zoster virus), rubella, cytomegalovirus (CMV), and herpesviruses (HSV) 1 and 2.
Recently,
the Zika virus (ZIKV) was identified as being transmissible vertically, adding
to the TORCH pathogens which have now become a focus of research once again.
The emergence of the Zika virus has reignited the need to address vertical
transmission.
Even in
developed countries, such as the US, infections with TORCH pathogens are linked
with severe disease in infants. Additionally, infection rates in developed
countries remain high, with up to 4,000 infants born in the US annually with
toxoplasmosis infections which can cause blindness, developmental delay, epilepsy
and more. Infections of the CMV virus are even more common, with 40,000 infants
born in the US each year with congenital infections of the virus which can
require complex surgical attention.
Signs and symptoms:
Subtle signs
such as an influenza-like illness, or possibly no symptoms at all. In such
cases, the effects may be seen first at birth.
Symptoms of
a vertically transmitted infection may include fever and flu-like symptoms. The
newborn is often small for gestational age. A petechial rash on the skin may be
present, with small reddish or purplish spots due to bleeding from capillaries
under the skin. An enlarged liver and spleen (hepatosplenomegaly) is common, as
is jaundice. However, jaundice is less common in hepatitis B because a
newborn's immune system is not developed well enough to mount a response
against liver cells, as would normally be the cause of jaundice in an older
child or adult. Hearing impairment, eye problems, mental retardation, autism,
and death can be caused by vertically transmitted infections.
During childbirth:
Babies can
also become infected by their mothers during birth. Some infectious agents may
be transmitted to the embryo or fetus in the uterus, while passing through the
birth canal, or even shortly after birth. The distinction is important because
when transmission is primarily during or after birth, medical intervention can
help prevent infections in the infant.[citation needed]During birth, babies are
exposed to maternal blood, body fluids, and to the maternal genital tract
without the placental barrier intervening. Because of this, blood-borne
microorganisms (hepatitis B, HIV), organisms associated with sexually
transmitted diseases (e.g., Neisseria gonorrhoeae and Chlamydia trachomatis),
and normal fauna of the genitourinary tract.
TORCH infection during pregnancy:
TORCH infections are the term given to a group of infectious diseases that can be passed to your baby during pregnancy, at delivery or after birth. TORCH stands for toxoplasmosis, rubella, cytomegalovirus, herpes and other agents.
Diagnosis:
When physical
examination of the newborn shows signs of a vertically transmitted infection,
the examiner may test blood, urine, and spinal fluid for evidence of the
infections listed above. Diagnosis can be confirmed by culture of one of the
specific pathogens or by increased levels of IgM against the pathogen.
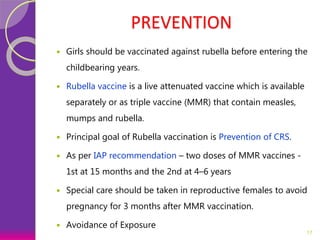
Prevention methods for
vertical transmission:
While more
research into the mechanism of vertical transmission is needed, there are
currently a number of preventative methods employed to reduce the vertical transmission
of pathogens. To prevent the vertical transmission of HIV, doctors test mothers
for infection with the virus and in the case of maternal infection, the best
practice involves controlling maternal infection, implementing prenatal
antiviral therapy and treating the mother and baby during labor and delivery,
delivering the baby by cesarean section rather than a natural birth.
Treatment:
Some
vertically transmitted infections, such as toxoplasmosis and syphilis, can be
effectively treated with antibiotics if the mother is diagnosed early in her
pregnancy. Many viral vertically transmitted infections have no effective
treatment, but some, notably rubella and varicella-zoster, can be prevented by
vaccinating the mother prior to pregnancy.
Pregnant
women living in malaria-endemic areas are candidates for malaria prophylaxis.
It clinically improves the anemia and parasitemia of the pregnant women, and
birthweight in their infants.
If the
mother has active herpes simplex (as may be suggested by a pap test), delivery
by Caesarean section can prevent the newborn from contact and consequent infection with this virus.
IgG2 antibody may play a crucial role in
prevention of intrauterine infections and extensive research is going on for
developing IgG2-based therapies for treatment and vaccination.[ntact, and
consequent infection, with this virusvoiding breastfeeding when possible.
Vertical transmission
of COVID-19:
Back in March 2020, the World Health Organization determined the COVID-19 outbreak to be a pandemic. To date, there have been more than 113 million cases confirmed in the laboratory and more than 2.5 million deaths have been attributed to COVID-19. While COVID-19 remains a significant threat to public health, its impact on infants born to infected mothers remains unclear.
Furthermore, whilst COVID-19 in newborns is rare, there have been cases of positive COVID-19 testing within 24 hours of birth (most of which have had mild or no symptoms). It is unknown whether newborns in these cases have contracted the virus before, during or post-birth.
This has led scientists to question whether SARS-CoV-2 could be transmitted vertically. While this was never documented in SARS-CoV and Middle East respiratory syndrome (MERS), far fewer people contracted these viruses so datasets may not have been large enough to detect it.
A recent paper, published in the journal Nature Communications in October 2020, has provided data that shows that babies born to SARS-CoV-2-positive women demonstrate elevated SARS-CoV-2-specific immunoglobulin G (IgG) and IgM antibody levels. This evidence suggests transference of the virus across the placenta, and, therefore, suggests vertical transmission occurred.
Additionally, a newer study, published in the American Journal of Obstetrics and Gynecology in January this year has revealed evidence that suggests that vertical transmission is most likely when the mother is infected during the third trimester. Again, further evidence is required to more thoroughly understand the nature of vertical transmission in COVID-19.
Overall, the
future prevention of vertical transmission of a range of viruses will heavily
depend on the research that is conducted going forward. There is a clear need
to protect children from vertical transmission in order to protect their
health. The emergence of COVID-19 may help to direct attention towards this
need, just as the Zika virus did.


Comments
Post a Comment