Menstrual Cycle Physiology
Menstrual Cycle Physiology
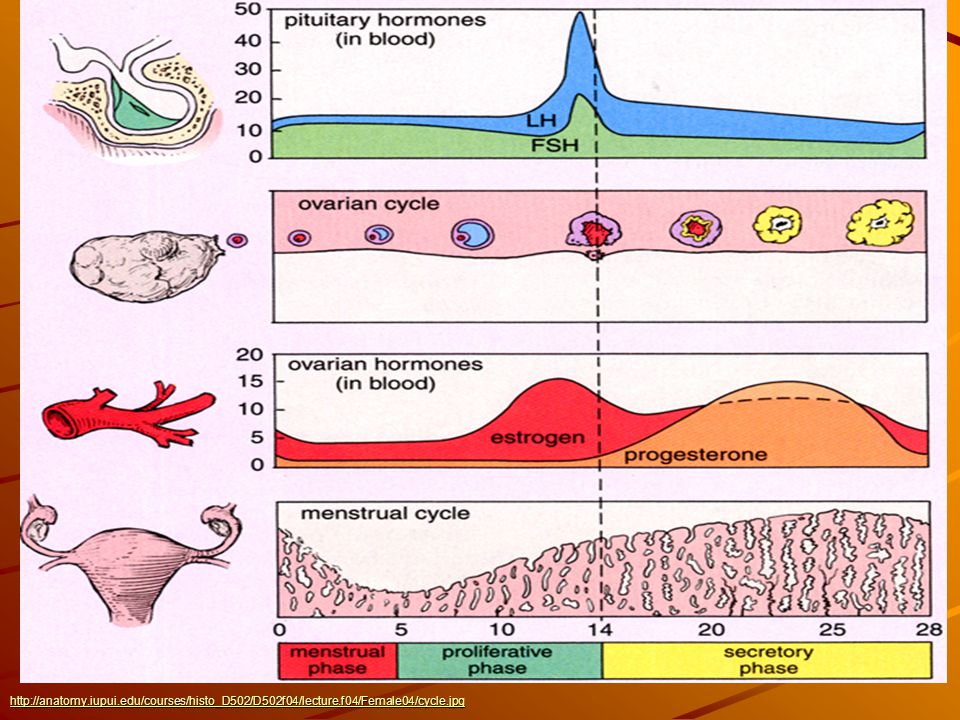
A normal menstrual cycle is the presence of regular vaginal bleeding. This occurs as a result of the shedding of the endometrial lining following failure of fertilization of the oocyte or failure of implantation. The cycle depends on changes occurring after puberty within the ovaries and fluctuation in ovarian hormone levels, which are themselves controlled by the pituitary and hypothalamus within the hypothalamo–pituitary–ovarian axis (HPO).
Hormones of
menstutral cycle:
The hypothalamus :
The
hypothalamus in the forebrain secretes the peptide hormone
gonadotrophin-releasing hormone (GnRH), which in turn controls pituitary
hormone secretion. GnRH
It must be
released in a pulsatile fashion to stimulate pituitary secretion of;
1. Luteinizing hormone (LH)
2. Follicle-stimulating hormone
(FSH).
The
pituitary gland:
GnRH
stimulation of the basophil cells in the anterior pituitary gland causes
synthesis and release of the gonadotrophic hormones FSH and LH. This process is
modulated by the ovarian sex steroid
hormones;
1. Oestrogen
2. Progesterone.
These hormones are released from ovaries by
response of LH and FSH.
Low levels of oestrogen have an inhibitory
effect on LH production (negative feedback), whereas high levels of oestrogen
will increase LH production (positive feedback).
Phases of menstutral cycle:
There are four phases of menstural cycle.
1. Mensturation
2. Follicular phase
3. Ovulation
4. Luteal phase
Mensturation:


Comments
Post a Comment