Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome
Polycystic
ovary syndrome (PCOS) is a condition in which the ovaries produce an abnormal
amount of androgens, male sex hormones that are usually present in women in
small amounts. The name polycystic ovary syndrome describes the numerous small
cysts (fluid-filled sacs) that form in the ovaries.
The
prevalence of polycystic ovaries seen on ultrasound isaround 25% of all women but is not always
associated with the full syndrome.
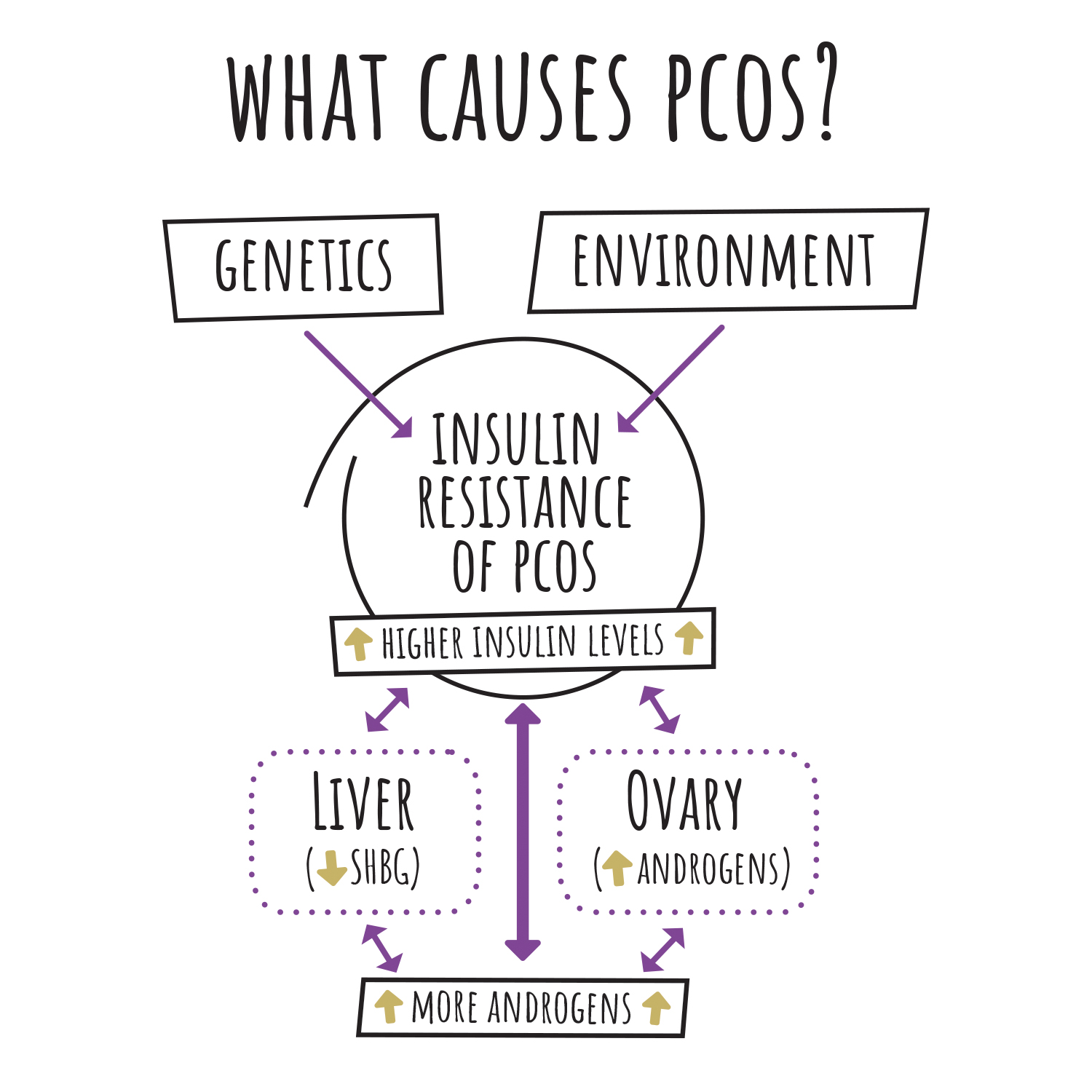
Etiology and Cause of PCOS
The
aetiology of PCOS is not completely clear, although the frequent familial trend
points to a genetic cause. The exact cause of PCOS is unknown. There is evidence
that genetics and several other factors play a role in causing PCOS: Higher levels of
male hormones called androgens: High
androgen levels prevent the ovaries from releasing eggs (ovulation), which
causes irregular menstrual cycles.
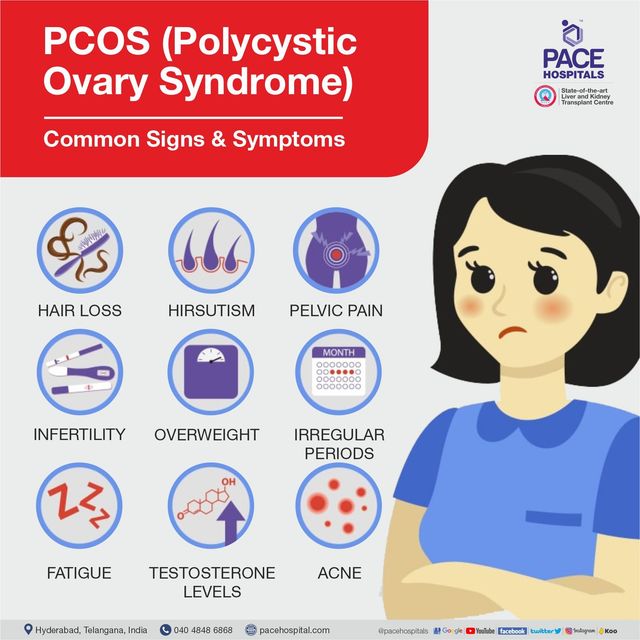
Clinical features of PCOs
•
Oligomenorrhoea/amenorrhoea in up to 75% of patients, predominantly related to
chronic anovulation.
• Hirsutism.
•
Subfertility in up to 75% of women.
• Obesity in
at least 40% of patients.
• Acanthosis
nigricans (areas of increased velvety skin pigmentation occur in the axillae
and other
flexures).
• May be
asymptomatic.
Diagnosis criteria for PCOS
Patients
must have two out of the three features below:
•
Amenorrhoea/oligomenorrhoea.
• Clinical
or biochemical hyperandrogenism.
• Polycystic
ovaries on ultrasound. The ultrasound criteria for the diagnosis of a
polycystic ovary are eight or more subcapsular follicular cysts <10 mm in
diameter and increased ovarian stroma. While these findings support a diagnosis
of PCOS, they are not by themselves sufficient to identify the syndrome.
Management of
PCOS
Management
of PCOS involves the following:
Medication for PCOS;
• Combined
oral contraceptive pill (COCP) to regulate menstruation. This also increases
sex hormonebinding globulin, which will help reduce androgenic symptoms.
• Cyclical
oral progesterone: used to regulate a withdrawal bleed.
•
Clomiphene: this can be used to induce ovulation where subfertility is a
factor.
• Lifestyle advice:
Dietary
modification and exercise is appropriate in these patients as they are at an increased
risk of developing diabetes and cardiovascular disease later in life. Aerobic
exercise has been shown to improve insulin resistance.
• Weight reduction.
Surgical treatment of PCOS:
• Ovarian
drilling, a laparoscopic procedure to destroy some of the ovarian stroma that
may prompt ovulatory cycles.
Treatment of hirsutism/androgenic symptoms of
PCOS:
• Eflornithine
cream (Vaniqua™) applied topically;
• Cyproterone
acetate (an antiandrogen contained in the Dianette™ contraceptive pill,
sometimes used alone);
• Metformin:
this is beneficial in a subset of patients with PCOS, those with
hyperinsulinaemia and cardiovascular risk factors. It improves parameters of
insulin resistance, hyperandrogenaemia, anovulation and acne in PCOS, and may
aid weight loss. It is less effective than clomiphene for ovulation induction and
does not improve pregnancy outcome;
• GnRH
analogues with low-dose HRT: this regime should be reserved for women
intolerant of other therapies;
• Surgical treatments (e.g. laser or electrolysis).
Home remedies for fertility and PCOs
1. It's also been found to help with fertility in some
cases of PCOS.
2. Chromium. Chromium supplements may improve your body
mass index, which can help with PCOS.
3. Cinnamon. Cinnamon comes from the bark of cinnamon
trees.
4. Turmeric.
5. Zinc.
6. Evening primrose oil.
7. Combined vitamin D and calcium.
8. Cod liver oil.


Comments
Post a Comment