Ectopic pregnancy
Ectopic pregnancy
Definition:
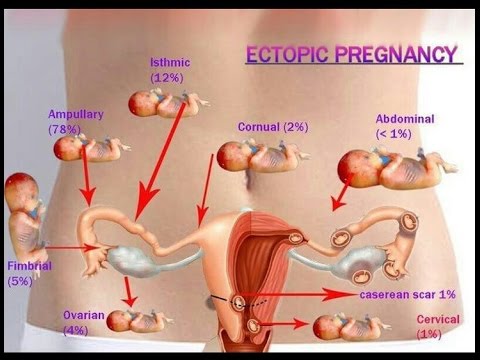
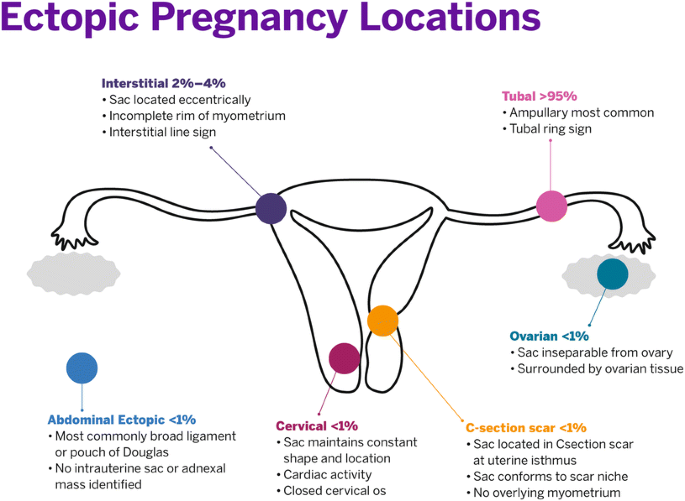
An ectopic pregnancy (EP) is defined as the implantation of a pregnancy outside the normal uterine cavity. Over 98% implant in the Fallopian tube. Rarely, ectopic pregnancies can implant in the interstitium of the tube, ovary, cervix, abdominal cavity or in caesarean section scars. A heterotopic pregnancy is the simultaneous development of two pregnancies: one within and one outside the uterine cavity.
Incidence and aetiology:
One in 80 pregnancies are ectopic. They account for 9–13% of maternal deaths in the Western world and 10–30% in low resource countries. The incidence of a heterotopic pregnancy in the general population is low (1:25,000–30,000), but significantly higher after in-vitro fertilization (IVF) treatment (1%) due to the transfer of two blastocysts.
Aetiological
factors for ectopic pregnancy:
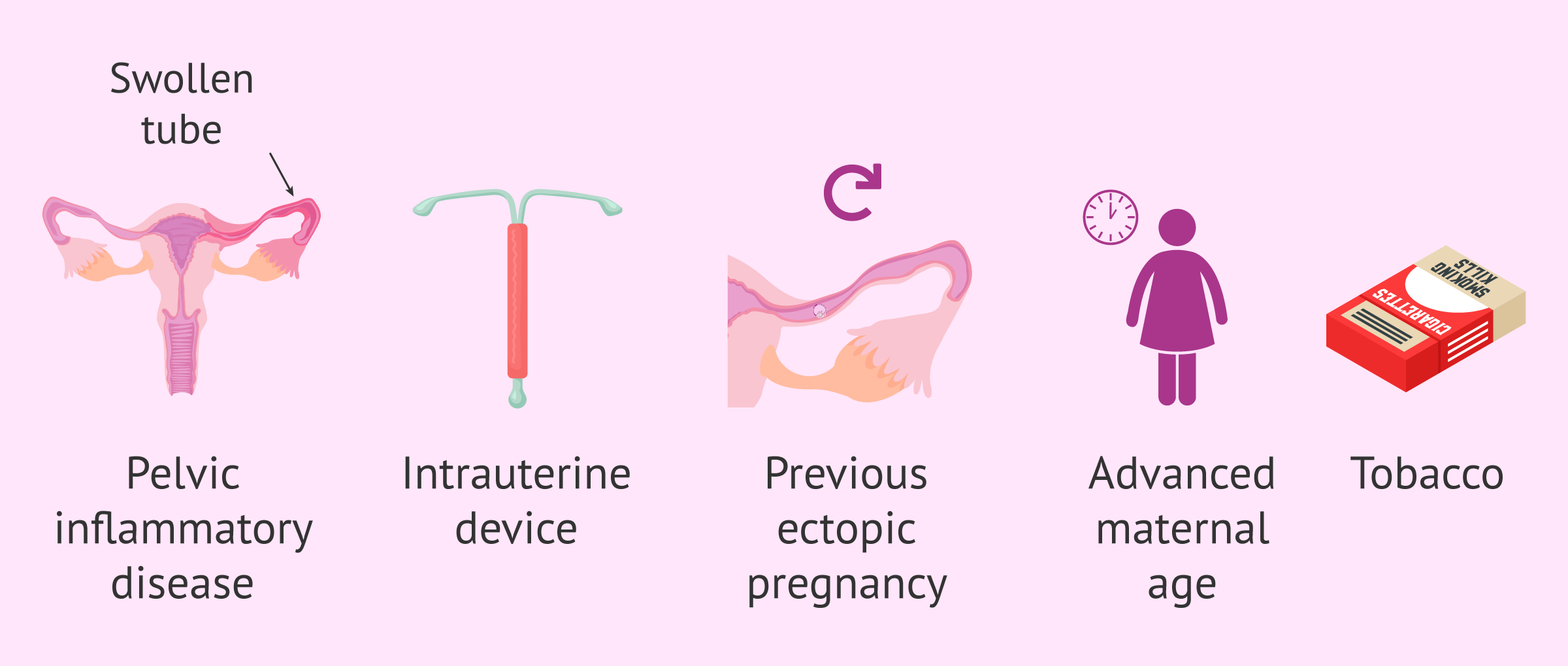
• Fallopian
tube damage due to pelvic infection (e.g. Chlamydia/Gonorrhoea), previous
ectopic pregnancy and previous tubal surgery.
• Functional
alterations in the Fallopian tube due to smoking and increased maternal age.
• Additional risk factors include previous
abdominal surgery (e.g. appendicectomy, caesarean section), subfertility, IVF,
use of intrauterine contraceptive devices, endometriosis, conception on oral
contraceptive/morning after pill.
Clinical
presentation of ectopic pregnancy:
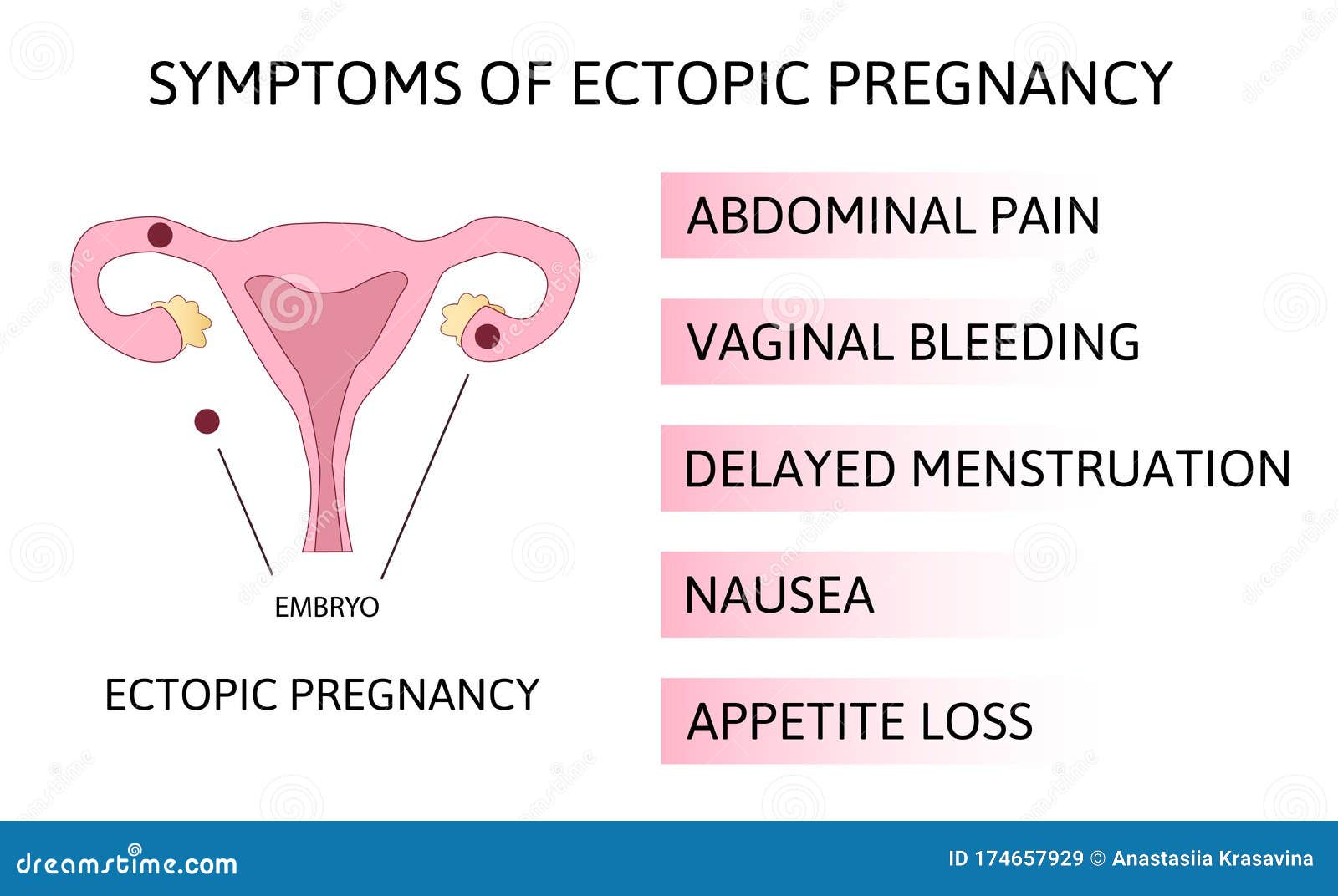
1. The majority of patients with an EP
present with a subacute clinical picture of abdominal pain and/or vaginal
bleeding in early pregnancy.
2. Rarely, patients present very acutely
with rupture of the EP and massive intraperitoneal bleeding.
3. The free blood in the peritoneal cavity can cause diaphragmatic irritation and shoulder tip pain.
The diagnosis of ruptured ectopic
pregnancy:
It is
usually clear as they present with signs of an acute abdomen and hypovolaemic
shock with a positive PT. It is, however, important to be aware that it is
common for women to experience bleeding or abdominal pain with a viable
intrauterine pregnancy.
Investigations of ectopic pregnancy:
The following are useful investigations for
the diagnosis of EP. Nonetheless, again, it is fundamentally important to
assess the woman clinically (‘ABC’, abdominopelvic examination) in conjunction
with the results of investigations to manage the patient.
• TVUSS:
identification of an intrauterine pregnancy (intrauterine gestation sac, yolk
sac +/− fetal pole) on TVUSS effectively excludes the possibility of an EP in
most patients except in those patients with rare heterotopic pregnancy. A TVUSS
showing an empty uterus with an adnexal mass has a sensitivity of 90% and
specificity of 95% in the diagnosis of EP. The presence of moderate to
significant free fluid during TVUSS is suggestive of a ruptured EP.
• Serum hCG:
the serum hCG level almost doubles every 48 hours in a normally developing
intrauterine pregnancy. In patients with EP, the rise of hCG is often
suboptimal. However, hCG levels can vary widely in individuals and thus
consecutive measurements 48 hours apart are often required for comparison
purposes.
•
Haemoglobin and ‘Group and Save’ (or cross-match if patient is severely
compromised):
• measure to
assess degree of intra-abdominal bleeding and rhesus status. Pregnancy of
unknown location
• In up to 40% of women with an EP the
diagnosis is not made on first attendance and they are labelled as having a
‘pregnancy of unknown location’ (PUL).
• A PUL is a working diagnosis defined as an
empty uterus with no evidence of an adnexal mass on TVUSS (in a patient with a
positive pregnancy test).
• The
mainstay of investigation of a PUL is consecutive measurement of serum hCG
concentrations.
An
endometrial biopsy can occasionally be helpful when hCG levels are static. All
PUL must be investigated to determine the location of the pregnancy.
Management
An EP can be managed using an expectant,
medical or a surgical approach, depending on clinical presentation and patient
choice.
Expectant management of ectopic
pregnancy:
Expectant management is based on the
assumption that a significant proportion of all EPs will resolve without any
treatment. This option is suitable for patients who are haemodynamically stable
and asymptomatic (and remain so). The patient requires serial hCG measurements
until levels are undetectable.
Medical management of ectopic
pregnancy:
Intramuscular
methotrexate is a treatment option for patients with minimal symptoms, an adnexal
mass <40 mm in diameter and a current serum hCG concentration under 3,000
IU/l. Methotrexate is a folic acid antagonist that inhibits deoxyribonucleic
acid (DNA) synthesis, particularly affecting trophoblastic cells.
The dose of
methotrexate is calculated based on the patient’s body surface area and is 50
mg/m2. After methotrexate treatment serum hCG is usually routinely measured on
days 4, 7 and 11, then weekly thereafter until undetectable (levels need to
fall by 15% between day 4 and 7, and continue to fall with
treatment).
Medical treatment should therefore only be offered if facilities are present
for regular followup visits. The few contraindications to medical treatment
include: (1) chronic liver, renal or haematological disorder; (2) active infection;
(3) immunodeficiency; and (4) breastfeeding. There aren also known side-effects
such as stomatitis, conjunctivitis, gastrointestinal upset and photosensitive
skin reaction, and about two-thirds of patients will suffer from non-specific
abdominal pain. It is important to advise women to avoid sexual intercourse
during treatment and to avoid conceiving for 3 months after methotrexate
treatment because of the risk of teratogenicity. It is also important to advise
them to avoid alcohol and prolonged exposure to sunlight during treatment.
Surgical management of ectopic
pregnancy:
The standard
surgical treatment approach is laparoscopy (Figure 5.3). Laparotomy is reserved
for severely compromised patients or where there are no endoscopic facilities.
The operation of choice is removal of the Fallopian tube and the EP within
(salpingectomy), or in some cases a small opening can be made over the site of
the EP and the EP extracted via this opening (salpingostomy). Salpingostomy is recommended
only if the contralateral tube is absent or visibly damaged, and it is
associated with a higher rate of subsequent EP. Pregnancy rates subsequently
remain high if the contralateral tube is normal because the oocyte can be
picked up by the ipsilateral or contralateral tube.


Comments
Post a Comment